By Emily Hightower RN, MSN and Holli White, MPS
Background
A quick search online will show that most individuals go into the field of nursing for similar reasons; the National Institutes of Health (NIH) sums it up nicely, citing nurses have “…a desire to serve others…a personal calling…and a desire to work in the [healthcare] field with the sick, in a noble and caring profession.” As a registered nurse who worked at the bedside for more than seven years, HDAI’s Emily Hightower, RN, CPN, MSN can attest that these are the same reasons she went into the field. Her passion for nursing propelled her through most of those years, despite demanding situations.
Her experience allowed her to work as a nurse in Haiti, Tanzania, and Malawi. While there are some vast differences among those countries and the United States, a common theme did emerge: nurses are short staffed and burned out everywhere.
Nursing is a highly respected field, and according to Nursing World it “has been ranked for 23 years straight as the most ethical and honest profession”. So, it begs the question…if nurses are honorable, ethical, and passionate, why are the rates of nurses fleeing the profession so high?

Burnout
Nurses and health care providers are vulnerable to burnout, defined as physical, emotional, and mental exhaustion. Burnout is a syndrome that results from poorly managed workplace stress. The World Health Organization states this may manifest as “feelings of energy depletion or exhaustion, increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job”. Unfortunately, burnout is continually on the rise. In a study published in the Journal of the American Medical Association, nearly 41% of nurses reported burnout in 2019, and by 2022 that number was a shade over 49%. Doctors fared similarly, reporting just under 32% in 2019 with a rise to 40% in 2022.
It is also worth mentioning that EMRs were meant to make nurses’ (and entire care teams’) lives easier. Instead, EMRs have inadvertently caused more work for clinicians by requiring them to add more and more data into the record, only to then have to sift through huge amounts of redundant information.
Burnout is not due to a lack of compassion; it is a byproduct of compassion fatigue. According to Nursing World, “providing compassionate care, working long hours, changing shift schedules, being on your feet for hours at a time, [and] staffing shortages are placing demands on nurses that are leading to burnout and driving them away from the bedside and into other roles.”
HDAI’s Emily Hightower is one of those nurses.
She left bedside nursing about three years ago, two years into the pandemic. With a young child at home, she needed something different that would give her longevity as a working mother, while still contributing to her family’s finances. She states, “I do still miss providing direct patient care, the people I worked with and the patients and families I connected with. However, none of these benefits were worth the long-term mental toll that was occurring. I personally know of at least six nurses, who graduated within the same two years as I did, who have left the bedside or are seeking out other career paths. Every one of these individuals went into the nursing field with high energy, passion, and a love for what they were doing. We must find a way to start taking care of our nurses before they are all gone.”
Burnout-induced staffing shortages – where does this leave us?
1. Public health crisis
Burnout can cause poor performance, which can lead to medical errors. It can also cause feelings of guilt and shame among providers. Burnout also means we will have fewer staff members as people leave the profession. According to a survey by staffing agency Incredible Health, 34% of nurses said they would leave their jobs by the end of 2022, with 44% saying that stress and burnout contributed to their decision.
We also know that depression and mental health concerns of our nurses is top of mind. CNN shared an article and references JAMA’s data, citing annual suicide rates across professions (per 100,000 person-years):
- 21.4 health care workers overall
- 16.0 registered nurses
- 12.6 non–health care workers
These are jarring statistics. Especially when you consider these are the same individuals who are working to better the mental and physical health of our nation.
The health care provider shortage is more than an inconvenience. It is a public health crisis. This crisis has been building since before the COVID-19 pandemic, but the pandemic exacerbated the situation. Healthcare providers experienced a shortage of supplies, an increased need for overtime shifts, and burdensome staffing shortages, all while attempting to manage their own illness or care for ill family members. Burnout has been exponentially increasing and while it’s terrible and has a negative impact on the lives of clinicians – what’s less talked about is that burnout ultimately impacts patient care, as well:
- Provider shortages in certain areas mean that large swaths of the population don’t have enough doctors or nurses to provide them with emergency care, treat their chronic illnesses, or deliver their babies.
- Health care staffing shortages lead to poor patient outcomes that can include hospital-acquired infections, patient falls and increased risk of death, according to the American Association of Colleges of Nursing.
- The Journal of Nursing Administration (JONA) cites that patients in understaffed units who experience two shifts understaffed are more likely to develop hospital associated infections (HAIs). In 2008, Medicare stopped payment to hospitals for three HAIs (catheter associated urinary tract infection, vascular catheter associated infection, and surgical site infection), directly impacting the health systems’ bottom line.
- The Joint Commission Journal on Quality and Patient Safety found similar results. In a review of 54 studies, they found that increased staffing is directly related to the decreased risk of acquiring Hospital Acquired Infection (HAIs).
- The European Journal of Cardiovascular Nursing states that higher staffing levels are associated with reduced mortality, medication errors, ulcers, restraint use, infections, and pneumonia. A higher nurse staffing level decreased the risk of in-hospital mortality by a whopping 14%.
It also warrants mentioning that with nurses leaving their careers prematurely in droves, there will be fewer seasoned nurses at the bedside to train and educate incoming nurses. The lessons that can be passed down by these nurses cannot always be taught in school or through a textbook.
2. Additional operational costs
In addition to burnout being a driver of staffing shortages and subsequent public health troubles, it is also a significant driver of direct costs to the healthcare ecosystem.
Operational labor costs have skyrocketed since the pandemic. Due to the staffing shortage, hospitals rely on outside staffing solutions, such as hiring registered nurses and other temporary clinical staff through traveling staffing agencies. This is a huge opportunity for those willing to travel for work. RNs are in high demand and can earn double to triple what they make as on-staff clinical employees. A staggering $1.52 billion was paid out in 2022 for travel workers in Massachusetts hospitals alone. 77%, the bulk of this $1.52 billion figure spent on temporary labor, was for travel nurses. Massachusetts Health & Hospital Association cites $1.52 billion for FY 2022 as an overwhelming 610% increase compared to $204 million in FY 2019.
The American Hospital Association reported a 258% increase in overall hospital labor costs from 2019-2022. This is driven in bulk from hospitals’ reliance on contract staffing agencies and a considerable increase in overtime hours, by nurses and other staff. While commendable, those staff who do remain in the field and work overtime to cover shortages, are more susceptible to burnout, which contributes to the cyclical burnout crisis.
To further complicate the cost conundrum, what does this mean for hospital profit margins and consumers – patients – down the road? Becker’s published a compelling article recently interviewing healthcare leaders and getting their insights on the question.
“‘The ultimate impact here is it will drive up the overall cost of care,’ Marvin O’Quinn, former president and COO of Chicago-based CommonSpirit, told Becker’s during a July podcast. ‘There’s no avoiding that. As the unit cost goes up, that cost at some point is going to have to be passed on.’
Stephen Klasko, an adviser at General Catalyst and the former CEO of Philadelphia-based Jefferson Health, and Robert Pearl, MD, former CEO of Kaiser’s Permanente Medical Group, echoed that sentiment.
‘It’s ridiculous to say in an algebraic way that if [labor costs] go up 20 to 25% that it’s not going to have an effect on either my ability to survive or coming up with some way that healthcare is going to get more expensive. That’s a fact,’ Mr. Klasko told Becker’s.
‘Nursing costs are no different than any other cost,’ Dr. Pearl, MD, a professor at Stanford (Calif.) University School of Medicine, told Becker’s. ‘With everything we do that adds cost, it either gets passed on to the insurer or to the patient.’”
We see a ripple effect with secondary cost impacts as well. Reduction in quality of care, such as an increase in HAIs as mentioned above, not only has a direct impact to patients, but can lead to payment penalties. A quick search highlights which hospitals are penalized by Medicare for high rates of complications (hospital-acquired conditions) or excess readmission rates.
Reducing nursing burnout and improving efficiencies in a digital ecosystem
1. AI, technology, and data-driven practices
It’s next to impossible to read much in healthcare tech news without seeing AI mentioned, and for good reason. When used responsibly, AI in healthcare can help to enhance clinical workflows through efficiencies — efficiencies that may help reduce medical errors and burnout. These improvements help enhance patient care, as well.
Interoperability, powered by AI, can create synergy across staff, an improvement in nurse/patient or nurse/care team communication, and a more streamlined health information ecosystem. Having easily accessible, readily surfaced, and prioritized patient data can lessen the strain on those using it. AI can help across the care continuum, from administrative tasks to automated updates for families regarding care plans and patient progress – all aiding nurses (and the rest of the care team) to work at the top of their licensure.
In a February 2024 article, How generative AI can help address the critical nursing shortage, Jill M. Lashay, healthcare attorney, states “AI can be used to assist nurses with clinical documentation and administrative tasks, making their work experience less stressful and more focused on their chosen vocation – patient care. This may result in higher recruitment and retention of nurses.” Her colleague, Carly Barnes, says “AI cannot be used to replace a nurse’s clinical experience, emotional support, or medical judgment, but can be used to push out patient medication reminders, assist with scheduling and billing, and help answer medical questions. Other advances in technology can also be used to help with medication dispensation and shelf stocking.”
Our company, Health Data Analytics Institute (HDAI), uses machine learning, generative AI, and foundational models to distill billions of national encounters and EMR data into one page of patient-level information that has insights that are actionable. We work to help providers surface data with technology, instead of being buried in data and wasting time searching in the EMR.
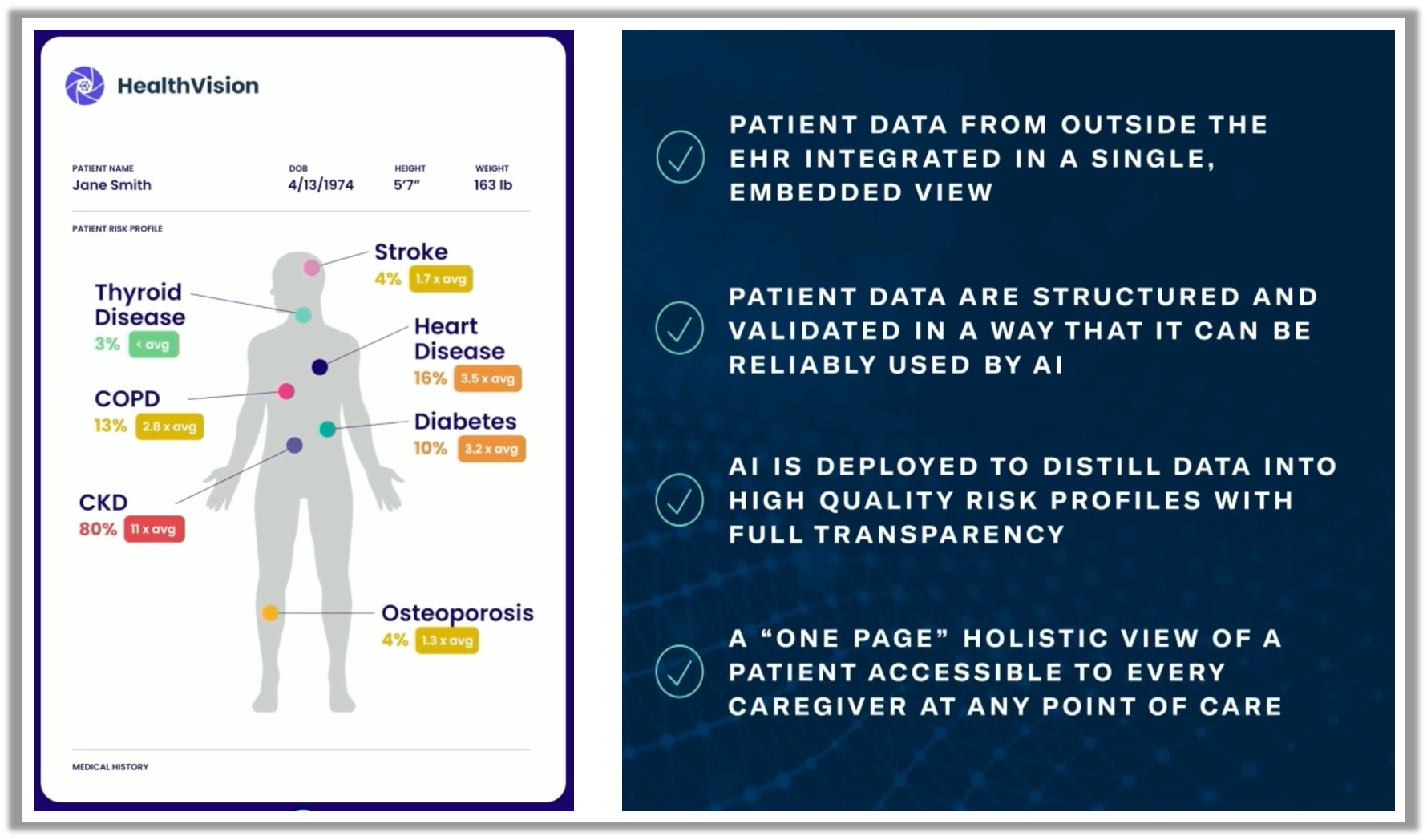
HealthVision transforms and synthesizes into a clinician-friendly, shared page - the Spotlight
At Houston Methodist, we leverage generative AI with our own governance wrapper around it to interpret every note that is written in the Houston Methodist system in real time. We extract millions of codes, pulled via analyzing millions of notes, and use this information to integrate both structured and unstructured data together (including data that’s new or historical). We generate the most comprehensive patient-level risk profiles possible, as well as lists of populations, in real time and keep them current as care progresses through the system, saving time and ensuring the most current and actionable data is surfaced. Predictive models and risk scores aid in quality of care and in improving efficiencies for staff.
In February of 2024, Houston Methodist published Utilizing Telenursing to Supplement Acute Care Nursing in an Era of Workforce Shortages. “In 3 months, almost 9,000 (67%) of patient admissions and discharges were conducted by an acute care telenurse, saving the bedside nurse an average of 45 minutes for each admission and discharge. Preliminary benefits to the program included more uninterrupted time with patients, more complete hospital admission and discharge documentation, and positive patient and nurse feedback about the program.” This is another example of utilizing new technology to save nursing staff time, improve efficiencies, and reduce burnout.
2. Cultural transformation and nursing retention
Investing in your team through positive work culture will never go out of style. Technology is critical in the workforce, but there is a human element involved and positive organizational culture trickles down from the top levels of leadership. Harvard shares the importance culture plays in long-term job satisfaction and quotes, “A poor workplace culture can negatively impact a person’s wellbeing. It can also significantly impact the company’s bottom line, leading to low productivity and high turnover.”
Ardent Health Services recently shared how they hired and retained 32% more permanent nurses in just one year. Their Chief Human Resources Officer, Carolyn Schneider, shared her cultural strategies in a recent webinar and highlights talent development as a key focus area. By focusing on developing talent, rather than just acquiring it, she is honing in on streamlining processes and creating a culture heavily invested in nursing education. Ardent’s retention strategies also increased employee loyalty.

Looking forward
Reduction in nursing burnout will have a direct, positive impact by:
- Improving the quality-of-care patients receive, arguably systematically improving clinical outcomes, patient satisfaction, and population health.
- Increasing the longevity of our nurses in their profession, propelling the vocation through mentorship and clinical expertise of seasoned nurses.
- Improving the financial strength of the healthcare ecosystem by restoring the balance in labor costs and potentially reducing reimbursement penalties from payers.
If we don’t get to the root of the problem and solve that, we will continue to experience nurses leaving the bedside for alternative roles or desiring to leave the field altogether. It is paramount that we find a way to support our healthcare workers and alleviate the burnout they are experiencing.
There is hope and a potential way to lighten the load through informatics and technology. Artificial intelligence (AI) can track and synthesize large amounts of patient data more efficiently than humans can. With that knowledge, we can enable organizations to connect the dots on information that previously may not have been utilized to understand a patient’s overall health status. Not only that, but we are quite literally able to find that “needle in a haystack patient” which can save providers time, save on overall spending, and ultimately save a patient’s life by better managing their chronic diseases. Integrating this technology into the day to day of bedside nurses and care managers could take the form of modified workflows, a different prioritization of patients, and an increase in preventative care. These changes can positively impact staffing ratios by enabling more time for nurses to spend on direct patient care.
The overall goal is to reduce the daily burden that is taking time and attention away from optimal care delivery. Some may fear technology advancements will reduce the need for nurses. This is not true. Using AI responsibly means that AI generated predictors and indicators must be coupled with nurses’ clinical judgement.
Our hope is that we all continue to gain awareness of these tools, so they can be implemented at the system level of our hospitals and become a baseline standard of care. When done the right way, AI can enable providers of all disciplines, be it patient care assistants, nurses, or physicians, to have more time at the bedside and with direct patient care. By better enabling our nurses, we can take better care of our patients, and that is what we are truly after in healthcare.
Contact us!
If you would like to discuss your work in the healthcare space and learn more about HDAI, please reach out to [email protected]. We would love to speak with you.
References
https://academic.oup.com/eurjcn/article/17/1/6/5925020
https://www.healthcarefinancenews.com/news/hospitals-labor-costs-increased-258-over-last-three-years
https://www.healthcareitnews.com/news/how-generative-ai-can-help-address-critical-nursing-shortage
https://kffhealthnews.org/news/hospital-penalties/
https://www.mhalink.org/news/hospital-temporary-labor-costs-a-staggering-1-52-billion-in-fy2022/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10160712/
https://nursejournal.org/articles/nurses-ranked-the-most-trusted-profession-2023/
https://pubmed.ncbi.nlm.nih.gov/31000210/
https://pubmed.ncbi.nlm.nih.gov/31752859/
https://www.sciencedirect.com/science/article/pii/S155372501730538X?via%3Dihub%5C
SHARE
