By Scott Cullen, MD – Chief Medical Officer at Health Data Analytics Institute
CMS is taking new steps to control rising healthcare costs. They believe some large Medicare Advantage insurers are “gaming” the coding system to increase payments. CMS recently proposed a major change: diagnoses would only count toward risk scores if they are directly related to the billed encounter. It’s unclear whether this approach will later apply to traditional Medicare, but it is important to watch.
Risk scoring is supposed to measure how complex a patient is to manage. It helps ensure fair payment for providers and fair comparisons across patient populations. Today, risk scores depend on all documented diagnoses, not just the ones relevant to a specific visit.
Chronic conditions are common. About 12.3% of Americans have four or more chronic illnesses. Nearly 79% of Medicare age patients have at least two conditions, most often hypertension and high cholesterol. These are meaningful risks, especially as cardiovascular disease is now the leading cause of death.
There are valid reasons to question retrospective chart reviews that aim to boost coding and reimbursement, especially in Medicare Advantage, where private insurers capture significant profits.
However, our research shows that prospectively identifying comorbidities has strong clinical value, independent of financial benefits. Using CMS’s Virtual Research Data Center, we analyzed case mix index (CMI), mortality, and follow-up rates across 118 major academic medical centers.
We found that hospitals in the top 20% for condition coding had 10% lower than expected mortality, as long as they also achieved at least an average 14-day post discharge follow-up. More importantly, 63% of this mortality difference came from clinical performance, not from inflated coding that raised “expected” risk. Better coding alone did not drive the improved outcomes.
Why might this be? Better condition recognition often means earlier and more coordinated clinical action. Stronger communication across teams leads to earlier detection, better monitoring, and faster intervention.
In response, HDAI has expanded our predictive modeling work with several leading AMCs. We are applying a subset of our 1,100 models to 180 high risk conditions that require first hour recognition. These predictions support clinical care and highlight valid CC and MCC coding opportunities. Because the model is prospective, the entire care team is alerted early, strengthening CDI and documentation efforts from Day One. The highest performing CMI institutions capture these codes both earlier and more consistently.
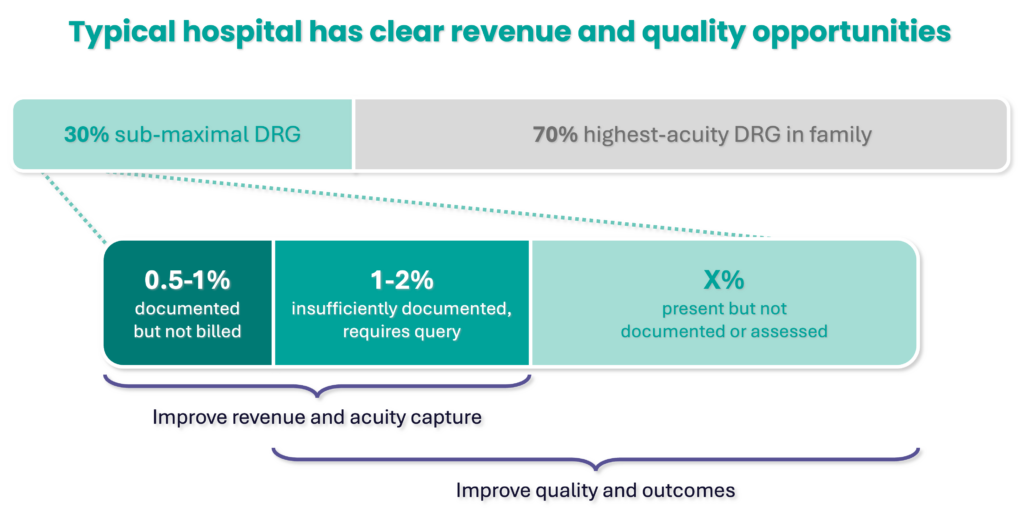
Given CMS’s direction and the financial strain on health systems, predictive approaches are becoming essential. The ability to retrospectively fill in codes is declining. Recent pilots show a 1.5–3% revenue opportunity for top tier institutions, with even greater upside for hospitals outside the top 100.
More details are coming soon. In the meantime, please reach out if you’d like to learn how our Predictive Diagnostic Discovery tools are improving both outcomes and revenue.
SHARE
